Robotic Ureteral Reconstruction
Minimally Invasive Approach to Ureteral Stricture Disease
How Is A Repair Done?
A ureteral reimplant surgery is a procedure that is in the lower part of the ureter. During the surgery, the surgeon removes any diseased part of the ureter and "re-implants" the ureter, fixing the connection to the bladder. A robotic ureteral implant is a surgery that involves the use of minimally-invasive robotic technology to make small incisions in the abdomen to repair the connection between the ureter and the bladder. The exact type of repair and the options available to you will be discussed in detail at the time of the consult.

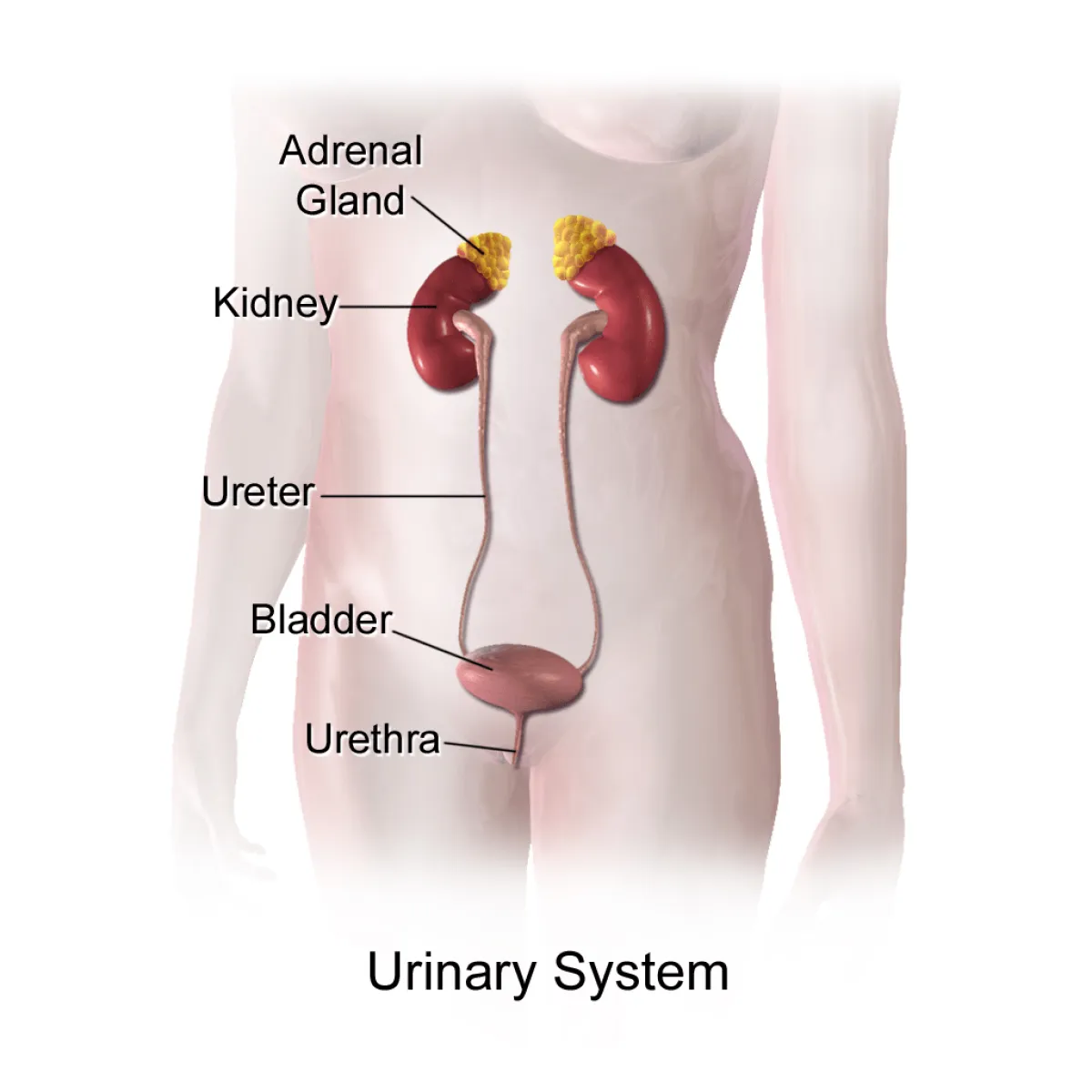
What is the Ureter?
The ureter is designed so that urine that the kidney makes enters the bladder, and does not allow it to flow back up into the kidney. Sometimes the ureter can become blocked from scar tissue, cancer, or other causes. Other times, you can have kinking and blockage caused by something on the outside of the tube. You may also have segments of the ureter itself not functioning to move the urine along.
Radiographic studies (ultrasound, CT scan, MRIs etc) should be performed initially with the goal of determining the location of the narrowing and the functional significance of the obstruction.
Schedule Reconstruction Appointment
The Operative Journey

Before Your Operation
7 Days Prior to Robotic Surgery
- STOP Aspirin, Ibuprofen, Coumadin/Warfarin, Plavix, Vitamin E after discussion with your surgeon
3 Days Prior to Robotic Surgery
Start enhanced recovery after surgery (ERAS) medications
- This is a patient centered, evidence based pathway to help reduce a patient's surgical stress response, optimize physiologic function, and facilitate recovery after the surgery
- These medications will be a combination of scheduled and on demand to help minimize pain and to avoid the use of narcotics in the post-operative setting
1 Day Prior to Robotic Surgery
- Nothing to eat or drink 12 hours ahead of the surgical start time
- There is no special diet that you need to be on prior to surgery
During Hospital Stay
- Length of stay: The length of hospital stay for most patients is approximately zero to one day.
- Diet: You can expect to have an intravenous (IV) catheter in for one to two days. Most patients are able to tolerate small sips of liquids a few hours after surgery and regular food the next day.
- Postoperative pain: Pain medication can be controlled and delivered by the patient via an injection (pain shot) administered by the nursing staff or by pills. You may experience some minor shoulder pain (one to two days) related to the carbon dioxide gas used to inflate your abdomen during the surgery. This will go away the more you move around after surgery.
- Nausea: You may experience some nausea related to the anesthesia or pain medication. Medication is available to treat persistent nausea.
- Urinary catheter: You can expect to have a urinary catheter draining your bladder (which is placed while you are asleep) for approximately one to two days after the surgery. It is not uncommon to have blood-tinged urine for a few days after surgery.
- Drain: You may have a drain coming out of a small incision in your side. This drain is placed around the operative site to prevent blood and fluid from building up around the repair. The drainage typically appears blood-tinged. It is usually removed the day the urinary catheter is removed. Sometimes, you may have to go home with the drain and have it removed in your doctor's office.
- Fatigue is common and should subside within a few weeks following surgery.
- Incentive spirometry: You will be expected to do some very simple breathing exercises to help prevent respiratory infections by using an incentive spirometry device (these exercises will be explained to you during your hospital stay). Coughing and deep breathing are an important part of your recuperation and help prevent pneumonia and other pulmonary complications.
- Ambulation: Once the surgery is completed, it is very important to get out of bed and begin walking under the supervision of your nurse or family member to help prevent blood clots from forming in your legs. You can expect to have sequential compression devices (SCDs) along with injections to help prevent blood clots from forming in your legs.
- Constipation/gas cramps: You may experience sluggish bowels for several days following surgery as a result of the anesthesia. Suppositories and stool softeners are usually given to help with this problem. Taking a teaspoon of mineral oil daily at home will also help to prevent constipation. Narcotic pain medication can also cause constipation, and therefore patients are encouraged to discontinue any narcotic pain medication as soon after surgery as tolerated.

Post-operative Recovery
- Pain control: You can expect to have some pain that may require pain medication for up to a week after discharge. Tylenol should be sufficient to control your pain. It is important to stay ahead of the pain.
- Showering: You may shower after returning home from the hospital. Your wound sites can get wet but must be padded dry immediately after showering. Do NOT scrub the incisions, let soap and water run down over them. Tub baths are not recommended in the first two weeks after surgery as this will soak your incisions and increase the risk of infection. The sutures underneath the skin will dissolve on their own in four to six weeks. The skin glue will fall off over the course of 1-2 weeks.
- Activity: Taking walks is advised. Prolonged sitting or lying in bed should be avoided. Climbing stairs is encouraged but should be taken slowly. Driving should be avoided for at least one to two weeks after surgery. Absolutely no heavy lifting (greater than 20 pounds) or exercising (jogging, swimming, treadmill, biking) until instructed by your doctor. Most patients return to full activity on an average of three weeks after surgery. You can expect to return to work in approximately two to four weeks.
- Follow-up appointment: You will see us in the office 1 week after your surgery. You may either call for a follow-up or one will be scheduled for you.
- Stent follow-up: If a stent is placed, then the stent will remain in place for approximately one month and will then be removed in the doctor's office through a cystoscope (a small telescoped passed down the urethra to retrieve the stent). It is not uncommon to feel a slight amount of flank fullness and urgency to void, which is caused by the stent. These symptoms often improve over time.
Why Choose Advanced Urology?

Comprehensive Care
We have ultramodern purpose built facilities to provide all your care. You will have access to every Super specialist at Advanced from recurrent urinary infections to clinical trials to the most challenging prostate cancer cases. We have all the expertise in house to help you.

The Advanced Difference
Advanced Super Specialists are board certified urologists with exceptional training. They focus on a narrow subset of urology. This superspecialization on a disease state leads to to more experience, greater expertise, and a better outcome. Our experts are world renown for their skill, knowledge, and compassion.

A Winning Team Committed to You
Our award winning team will collaborate with you, your family, and the other providers involved in your care. We think communication is essential in delivering great outcomes. The most important thing to know is that we are here for you.
Specific Complications
- Injury to the ureter or surrounding structures requiring additional surgery to repair the injury (<1%).
- An abnormal connection between channels in your body (fistula).
- Stent related discomfort- Discomfort could include: blood in the urine, pain or pressure with urination, and/or frequency and urgency of urination.
- A urinary leak may occur- This will generally require the stent to remain in for longer. Sometimes a tube is also placed in the back. The leak will often heal by itself.
- Scaring at the anastomosis This may require a second procedure to fix the scar tissue.

Advanced Techniques
Better Outcomes & Less Side Effect
- Grafts
- Outpatient Robotic Surgery with Enhanced Recovery Pathway
- Ureteral substitution with intestine