Robotic Surgery
The Best Robotic Surgery Program in Atlanta
We provide a comprehensive approach to treat all of our patient's needs. We can provide the least disruption to your life without sacrificing outcomes. Our physicians provide state-of-the-art care utilizing advanced techniques. See how we are different from other groups. We offer same-day surgery at our cutting edge surgery center to help minimize disruption to your busy life. We offer consultation with fellowship trained robotic surgeons, multi-disciplinary approach including multiple modalities for treatment.
What are the Benefits of Robotic Surgery?
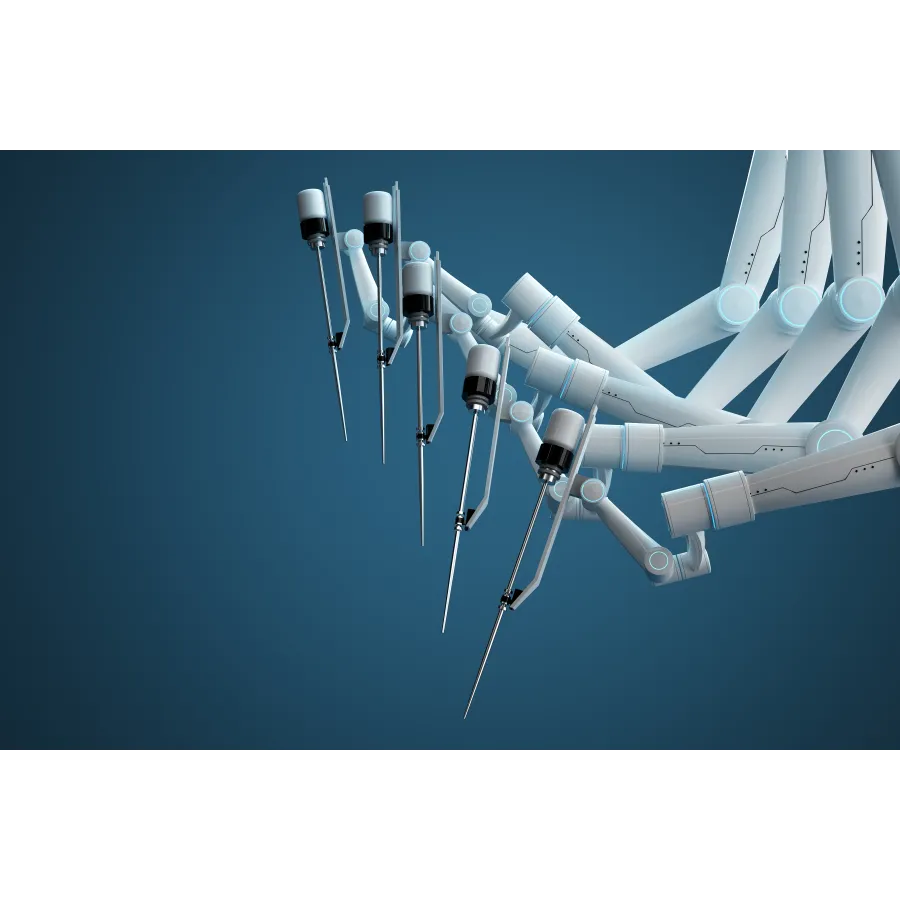
Robotic surgery involves utilizing small incisions (~8mm) to allow for robotic arms to be inserted. During the operation, the surgeon sits at an operating console and controls the instruments. The robot arms hold the instruments and the surgeon moves them while sitting at the console.
The robot is unable to move on its own. The robotic system allows for improved vision due to the 3d magnified vision. The arms also allow for precise, accurate movements in spaces that were physically not possible in the era of open surgery.
- Less pain and discomfort
- Quicker recovery time and faster return to your normal activities
- Shorter hospital stay
- Less scarring than open surgery
- Less chance of complications
- Less blood loss
- Less risk of infection
Prostate Conditions

Robotic Radical Prostatectomy (Prostate Cancer)

Robotic Salvage Prostatectomy (Surgery after Radiation for contained Prostate Cancer)

Robotic Simple Prostatectomy (Very Enlarged Prostate causing urinary difficulties)
Robotic Surgery: Prostate FAQ's
What are the treatment options for prostate cancer?
There are multiple options when it comes to treating localized prostate cancer:
- Watchful Waiting or Active Surveillance For select patients, they can avoid any intervention for low grade prostate cancer. In these patients, the risk of progression is not zero, but it is low. Surveillance usually consists of PSA monitoring, imaging, and periodic biopsies every one to two years or so. This option is more appropriate for older men, men with decreased life expectancy, medical problems making treatment unsafe, or men with less aggressive cancers that are less likely to progress.
- Surgery This treatment option involves removal of the prostate and the lymph nodes around the prostate.
- Radiation This is performed by a radiation oncologist. Different types of radiation are available based on patient factors and preferences.
- Hormonal Therapy This may be used in addition to the other treatments. It is usually not used as a solitary treatment option.
- Other Therapies These include things such as high-intensity focused ultrasound (HIFU), cryotherapy (freezing) and proton therapy.
What are the specific benefits/risks of surgery versus radiation?
Surgery and radiation can be equivalent options for many people, with the deciding factor being personal preference.
Prostate specific considerations include:
- Radiation can affect urinary symptoms temporarily and sometimes even over a long time frame. In patients who have severe urinary symptoms at baseline, surgery may be a better option as that will often relieve some of the urinary symptoms.
- Some treatment modalities like brachytherapy also have a size requirement to allow for optimal seed placement. This is not a limitation for surgery.
- Some people may be unfit for surgery and in those scenarios, radiation is a very good option. One thing to note is that there is no age limit for surgery, as this depends more on health than actual age.
- Another consideration is to think about what would happen if the primary treatment fails. While this would not be a best case scenario, the fact of the matter is that some subset of patients will experience a recurrence. If the recurrence is elsewhere in the body and not near the prostate, then they would have the option of hormonal therapy as a common first therapy. However, if they recur locally:
- If radiation fails, a few options remain. While surgery (called salvage prostatectomy) may be possible after radiation, it is much harder and fraught with increased complications. It is only performed in selective cases and by a smaller number of urologists around the country. The risks of this surgery would need to be discussed in detail with your urologist.
- If surgery fails locally, radiation can still be given. Many may feel comfortable knowing that a 2nd line option is still available should surgery fail as opposed to a higher risk surgery if radiation fails. But again, most cancers will not need another treatment, unless they are more aggressive or advanced cancers.
Personal considerations include:
- Some men do not like idea of surgery because of anesthesia, pain or scarring that may occur. With the enhanced recovery after surgery pathway, most people have minimal pain and scarring.
- The level of information gleaned from surgery is different than radiation.
- In surgery, because we remove the entire prostate and lymph nodes, we are able to tell if the biopsy gleason grade is the same. In about 25% of cases, the final gleason score is worse than the one on the biopsy. We are also able to tell if cancer has microscopically spread to the lymph nodes. Also, the PSA should become undetectable after surgery if it all the cancer has been contained. Some men also feel better knowing that the cancer has been physically removed from the body.
- With radiation, we do not get any more pathology information other than what was evident on the biopsy. The PSA is also tougher to track after radiation because it can fluctuate since the prostate is still left in the body.
- The timing of the side effects.
- With surgery, the side effects of treatment are up front. With radiation they tend to come weeks to months later and vary in severity and duration from person to person. There is also an increased risk of secondary cancers with radiation. Generally, in people who are young and healthy, surgery is the more preferred approach.
What are the side effects from surgery?
While transient, the two main issues from surgery are:
- Incontinence - leakage of urine, either continued or with stress such as a cough or exercise
- Most men will require a diaper or pad once the catheter comes out. This will get better over time, especially if performing Kegel exercises or doing pelvic floor physical therapy on a regular basis. Most improve by 1 to 3 months, but sometimes can take up to 6 months.
- Erectile Dysfunction
- The level of dysfunction depends on baseline erectile function prior to surgery. Generally, the better function that you start with, the more likely you are to regain that function. Also, aggressiveness of nerve sparing will factor into this. Typically this lasts 6 to 12 months after surgery.
What are the side effects of radiation?
The goal of radiation is to kill all the cancer cells in the prostate. In order to reach the appropriate doses in the prostate, some of the radiation will have effect on the other organs around the prostate, most commonly the bladder and rectum. The nerves that allow erections for sexual function are also impacted. The severity and duration of side effects depend on the radiation technique and the sensitivity of the individual patient.
Long-term effects can include:
- Urinary effects - urgency of urination, burning with urination, blood in the urine,
- Bowel effects - diarrhea, painful bowel movements or blood in the stool.
- Some patients can develop severe inflammation and scarring of the urethra or rectum that can last months to years or require surgical intervention.
- There is also an increased risk of cancers of the rectum or bladder.
What does nerve sparing mean?
Normally, nerves that help with urinary control and ones that are necessary for erections all run alongside the prostate towards the urethral sphincter. The amount of these nerves that can be spared will depend on the location of the prostate cancer and also the severity of it. Even with nerve-sparing, some men will not regain erections that are as good as before surgery. Some men may need medications to help achieve erections adequate for sex. Younger men and men with good erectile function before surgery typically have better results after surgery. Even if men are unable to have a natural erection, the sensation to the penis and the ability to orgasm will not be affected.
In the end, cancer control is the most important factor as there are other treatments available to help with erectile dysfunction after a radical prostatectomy.
What is the typical source for someone undergoing robotic surgery?
- Hospital stay: Most of the time, this can be done as a same day procedure.
- Diet: You can expect to start sips of liquids a few hours after surgery. Continue a liquid diet and slowly start advancing it as you pass gas on a more regular basis.
- Postoperative pain: Pain medication can be controlled and delivered by the patient via an injection (pain shot) administered by the nursing staff or by pills. You may experience some minor shoulder pain (one to two days) related to the carbon dioxide gas used to inflate your abdomen during the surgery. This will go away the more you move around after surgery.
- Nausea: You may experience some nausea related to the anesthesia or pain medication. Medication is available to treat persistent nausea.
- Urinary catheter: You can expect to have a urinary catheter draining your bladder (which is placed in the operating room while you are asleep) for approximately one week after the surgery. This will help the connection of the bladder to the urethra heal. It is not uncommon to have blood-tinged urine for a few days after surgery.
- Drain: You may have a drain coming out of a small incision in your side. This drain is placed in the operating room around the operative site to prevent blood and fluid from building up. The drainage typically appears blood-tinged. It is usually removed before you go home. If persistent high-volume drainage occurs, you may have to go home with the drain and have it removed in your doctor's office.
- Fatigue is common and should subside within a few weeks following surgery.
- Incentive spirometry: You will be expected to do some very simple breathing exercises to help prevent respiratory infections by using an incentive spirometry device (these exercises will be explained to you during your hospital stay). Coughing and deep breathing are an important part of your recuperation and help prevent pneumonia and other pulmonary complications.
- Ambulation: Once the surgery is completed, it is very important to get out of bed and begin walking under the supervision of your nurse or family member to help prevent blood clots from forming in your legs. You can expect to have sequential compression devices (SCDs) along with injections to help prevent blood clots from forming in your legs.
- Constipation/gas cramps: You may experience sluggish bowels for several days following surgery as a result of the anesthesia. Suppositories and stool softeners are usually given to help with this problem. Taking a teaspoon of mineral oil daily at home will also help to prevent constipation. Narcotic pain medication can also cause constipation, and therefore patients are encouraged to discontinue any narcotic pain medication as soon after surgery as tolerated.
What is the typical follow-up after surgery?
Typical follow-up includes the following:
- About 1 week after surgery, the catheter is removed and pathology will be discussed. You will need to start wearing diapers/pads.
- You will begin penile rehabilitation and pelvic floor physical therapy.
- At one month, follow up to assess improvement in incontinence and erections.
- At three months, we will review your first PSA blood test.
- Six months later and beyond, we will check your PSA every three months for the first year after surgery and then less frequently.
How many robotic surgeries has Advanced performed?
Our robotic physicians are fellowship trained to perform robotic procedures using state-of-the-art techniques. For some of them, their practice is limited to only robotic surgery. Collectively, they have performed over 2,500. They are also trained in open surgery should the need arise.
Where will the surgery be performed?
Depending on your risk profile and fitness level, it can either be performed as an outpatient surgery at one of our advanced surgery centers or at the hospital in the event that you will need to stay over.
We did not find your search. Please try another entry.
We did not find your search. Please try another entry.
Kidney Conditions

Robotic Radical/Total Nephrectomy (Large Tumors or Non-functioning Kidneys)

Robotic Partial Nephrectomy (Small Kidney Tumors and to save kidney function)

Robotic Retroperitoneal Partial Nephrectomy (Patients with small kidney masses with multiple intraabdominal surgeries)

Robotic Nephroureterectomy with Bladder Cuff (Upper tract urothelial/ureteral cancers)

Robotic Ureteral Reconstruction (Blockages of the ureter)
Robotic Surgery: Kidney FAQ's
What are the treatment options for a kidney mass?
Active Surveillance
About 15% of kidney tumors may be benign. Some tumors may also be very slow growing cancers that will never become life-threatening. For this reason, some patients may be actively followed with surveillance and periodic scans. This is most appropriate for older patients, those with less than a 5-year life expectancy, and those with medical problems making treatment unsafe or when the tumor appears more likely benign on scans.
Percutaneous Ablation
Some tumors can be treated by placing a needle into the tumor and then use this to freeze or burn the tumor. This treatment may not be possible in all masses. Also, this may have a lower cure rate than removing the mass.
Surgery
This treatment option involves removal of the tumors. Ideally, the kidney can usually be spared and only the mass may need to be removed. Sometimes the entire kidney is removed. Our surgeons at Advanced have performed hundreds of kidney and adrenal tumor removals robotically, without having to resort to traditional open surgery.
Radiation
Radiation is not an option to treat kidney tumors.
Newer Agents
Chemotherapy or immunotherapy agents are not used in the localized setting. These treatments are only used for cancers that have already spread to other parts of the body.
What are the benefits of a kidney robotic surgery?
Robotic surgery allows for a minimally invasive approach. The small incisions will be less painful, so patients are able to move around right away and can go home from the hospital faster. They are also able to return to their normal baseline at a much faster rate than open surgery. Robotic surgery also usually has less blood loss and decreased complication rate.
What is the typical course for someone undergoing robotic surgery?
- Hospital stay: The length of hospital stay for most patients is approximately one to two days.
- Diet: You can expect to have an intravenous (IV) catheter in for one to two days. (An IV is a small tube placed into your vein so that you can receive necessary fluids and stay well hydrated until you are able to tolerate a diet; it also provides a way to receive medication). Most patients are able to tolerate ice chips and small sips of liquids a few hours after surgery and regular food the next day. Once on a regular diet, pain medication can be given by mouth instead of by IV or shot.
- Postoperative pain: Pain medication can be controlled and delivered by the patient via an injection (pain shot) administered by the nursing staff or by pills. You may experience some minor shoulder pain (one to two days) related to the carbon dioxide gas used to inflate your abdomen during the surgery. This will go away the more you move around after surgery.
- Nausea: You may experience some nausea related to the anesthesia or pain medication. Medication is available to treat persistent nausea.
- Urinary catheter: You can expect to have a urinary catheter draining your bladder (which is placed in the operating room while you are asleep) for approximately one to two days after the surgery. It is not uncommon to have blood-tinged urine for a few days after surgery.
- Drain: You will have a drain coming out of a small incision in your side. This drain is placed in the operating room around the operative site to prevent blood and fluid from building up around the kidney and pyeloplasty repair. The drainage typically appears blood-tinged. It is usually removed the day the urinary catheter is removed. If persistent high-volume drainage occurs, you may have to go home with the drain and have it removed in your doctor's office.
- Fatigue is common and should subside within a few weeks following surgery.
- Incentive spirometry: You will be expected to do some very simple breathing exercises to help prevent respiratory infections by using an incentive spirometry device (these exercises will be explained to you during your hospital stay). Coughing and deep breathing are an important part of your recuperation and help prevent pneumonia and other pulmonary complications.
- Ambulation: Once the surgery is completed, it is very important to get out of bed and begin walking under the supervision of your nurse or family member to help prevent blood clots from forming in your legs. You can expect to have sequential compression devices (SCDs) along with injections to help prevent blood clots from forming in your legs.
- Constipation/gas cramps: You may experience sluggish bowels for several days following surgery as a result of the anesthesia. Suppositories and stool softeners are usually given to help with this problem. Taking a teaspoon of mineral oil daily at home will also help to prevent constipation. Narcotic pain medication can also cause constipation, and therefore patients are encouraged to discontinue any narcotic pain medication as soon after surgery as tolerated.
What should I do once home from surgery?
- Pain control: You can expect to have some pain that may require pain medication for up to a week after discharge. Tylenol should be sufficient to control your pain. It is important to stay ahead of the pain.
- Showering: You may shower after returning home from the hospital. Your wound sites can get wet but must be padded dry immediately after showering. Do NOT scrub the incisions, let soap and water run down over them. Tub baths are not recommended in the first two weeks after surgery as this will soak your incisions and increase the risk of infection. The sutures underneath the skin will dissolve on their own in four to six weeks. The skin glue will fall off over the course of 1-2 weeks.
- Activity: Taking walks is advised. Prolonged sitting or lying in bed should be avoided. Climbing stairs is encouraged but should be taken slowly. Driving should be avoided for at least one to two weeks after surgery. Absolutely no heavy lifting (greater than 20 pounds) or exercising (jogging, swimming, treadmill, biking) until instructed by your doctor. Most patients return to full activity on an average of three weeks after surgery. You can expect to return to work in approximately two to four weeks.
- Follow-up appointment: You will need to call the office after your surgery to schedule a follow-up appointment as instructed by your surgeon.
- Stent follow-up: If a stent is placed, then the stent will remain in place for approximately one month and will then be removed in the doctor's office through a cystoscope (a small telescoped passed down the urethra to retrieve the stent). It is not uncommon to feel a slight amount of flank fullness and urgency to void, which is caused by the stent. These symptoms often improve over time.
How many robotic surgeries has Advanced performed?
Our robotic physicians are fellowship trained to perform robotic procedures using state-of-the-art techniques. For some of them, their practice is limited to only robotic surgery. Collectively, they have performed over 2,500. They are also trained in open surgery should the need arise.
Where is the surgery performed?
Depending on your risk profile and fitness level, it can either be performed as an outpatient surgery at one of our advanced surgery centers or at the hospital in the event that you will need to stay over.
We did not find your search. Please try another entry.
We did not find your search. Please try another entry.
Robotic Surgery: Bladder FAQ's
What are the treatment options for an advanced bladder mass?
For treatment of patients with muscle invasive bladder cancer or aggressive bladder cancer, radical cystectomy (removal of the entire bladder plus the regional lymph nodes) remains the gold standard for treatment. Occasionally, nearby organs also have to be removed as well. In women, this may include removal of the cervix, ovaries, fallopian tubes, uterus and part of the vagina. In men, it may include removal of the prostate, seminal vesicles and part of the vas deferens.
What are the benefits of a robotic bladder surgery?
Robotic surgery allows for a minimally invasive approach. The small incisions will be less painful, so patients are able to move around right away and can go home from the hospital faster. They are also able to return to their normal baseline at a much faster rate than open surgery. Robotic surgery also usually has less blood loss and decreased complication rate.
The surgical robotic system also helps improve the ability to perform a lymph node dissection because of its superior range of motion and precise, controlled movements.
How is a robotic radical cystectomy peformed?
During the procedure, the patient's abdomen is inflated with gas and the robot's camera and operating arms are inserted through very small incisions in the abdomen. The surgeon then uses the robotic instruments to disconnect the bladder and any of the surrounding organs. These organs are then placed in a bag and usually removed either through the vagina or a low 2- to 3-inch incision that can be hidden in a skin crease. An extended pelvic lymph node dissection is also performed as part of the procedure. This will provide more accurate information about the stage of the cancer.
What are the different urinary reconstruction options?
Since radical cystectomy involves removal of the entire bladder, patients are required to undergo urinary reconstruction as part of the procedure. Our surgeons use cutting edge techniques to use tissue from the patient's intestine to create new ways of collecting the urine:
- Creation of an ileal conduit (urostomy) - incontinent diversion: In this approach, the surgeon uses part of the patient's intestine to create a channel that connects the ureters to a surgically created opening in the abdomen (stoma). Usually, the stoma is placed at one of the port sites so that no new incision is required. The urine continuously passes through the conduit and out the stoma into an external appliance.
- Creation of an orthotopic neobladder - continent diversion: In appropriate patients, an orthotopic neobladder may be fashioned from a larger piece of intestine to form a new "bladder." In this procedure, the ureters are attached at one end and the urethra at the other and the patient is able to pass urine out in the same way he or she did prior to surgery. There is no external appliance needed in this situation.
What is the typical course for someone undergoing robotic bladder surgery?
- Hospital stay: The length of hospital stay for most patients is approximately three to five days.
- Diet: You can expect to have an intravenous (IV) catheter in for one to two days. (An IV is a small tube placed into your vein so that you can receive necessary fluids and stay well hydrated until you are able to tolerate a diet; it also provides a way to receive medication). Most patients are able to tolerate ice chips and small sips of liquids a few hours after surgery. They will continue on a liquid diet until they start to pass more flatus. Once on a regular diet, pain medication can be given by mouth instead of by IV or shot.
- Postoperative pain: Pain medication can be controlled and delivered by the patient via an injection (pain shot) administered by the nursing staff or by pills. You may experience some minor shoulder pain (one to two days) related to the carbon dioxide gas used to inflate your abdomen during the surgery. This will go away the more you move around after surgery.
- Nausea: You may experience some nausea related to the anesthesia or pain medication. Medication is available to treat persistent nausea.
- Urinary catheter: Depending on the type of urinary reconstruction, you may have a urinary catheter draining your neobladder. This will likely stay in place for about 4 weeks to ensure complete healing. It is not uncommon to have blood-tinged or mucousy urine for a few days after surgery.
- Drain: You will have a drain coming out of a small incision in your side. This drain is placed in the operating room around the operative site to prevent blood and fluid from building up around the kidney and pyeloplasty repair. The drainage typically appears blood-tinged. It is usually removed the prior to discharge, unless there is urine leakage. If persistent high-volume drainage occurs, you may have to go home with the drain and have it removed in your doctor's office.
- Fatigue is common and should subside within a few weeks following surgery.
- Incentive spirometry: You will be expected to do some very simple breathing exercises to help prevent respiratory infections by using an incentive spirometry device (these exercises will be explained to you during your hospital stay). Coughing and deep breathing are an important part of your recuperation and help prevent pneumonia and other pulmonary complications.
- Ambulation: Once the surgery is completed, it is very important to get out of bed and begin walking under the supervision of your nurse or family member to help prevent blood clots from forming in your legs. You can expect to have sequential compression devices (SCDs) along with injections to help prevent blood clots from forming in your legs.
- Constipation/gas cramps: You may experience sluggish bowels for several days following surgery as a result of the anesthesia. Suppositories and stool softeners are usually given to help with this problem. Taking a teaspoon of mineral oil daily at home will also help to prevent constipation. Narcotic pain medication can also cause constipation, and therefore patients are encouraged to discontinue any narcotic pain medication as soon after surgery as tolerated.
What should I do once home from surgery?
- Pain control: You can expect to have some pain that may require pain medication for up to a week after discharge. Tylenol should be sufficient to control your pain. It is important to stay ahead of the pain.
- Fluid Management: You can very dehydrated after a surgery like this. So it is important to continue to drink as much fluid as you can. We will also set up a home health nurse to come give you IV hydration during the early weeks of recovery.
- Diversion Care: You will be given instructions on how best to care for the urinary reconstruction that you have. It is important to follow those directions to prevent urinary tract infections.
- Showering: You may shower after returning home from the hospital. Your wound sites can get wet but must be padded dry immediately after showering. Do NOT scrub the incisions, let soap and water run down over them. Tub baths are not recommended in the first two weeks after surgery as this will soak your incisions and increase the risk of infection. The sutures underneath the skin will dissolve on their own in four to six weeks. The skin glue will fall off over the course of 1-2 weeks.
- Activity: Taking walks is advised. Prolonged sitting or lying in bed should be avoided. Climbing stairs is encouraged but should be taken slowly. Driving should be avoided for at least one to two weeks after surgery. Absolutely no heavy lifting (greater than 20 pounds) or exercising (jogging, swimming, treadmill, biking) until instructed by your doctor. Most patients return to full activity on an average of three weeks after surgery. You can expect to return to work in approximately two to four weeks.
- Follow-up appointment: You will need to call the office after your surgery to schedule a follow-up appointment as instructed by your surgeon.
- Stent follow-up: The stents will remain in place for approximately one month and will then be removed in the doctor's office through a cystoscope (a small telescoped passed down the urethra or stoma to retrieve the stent). It is not uncommon to feel a slight amount of flank fullness and urgency to void, which is caused by the stent. These symptoms often improve over time.
How many robotic surgeries has Advanced performed?
Our robotic physicians are fellowship trained to perform robotic procedures using state-of-the-art techniques. For some of them, their practice is limited to only robotic surgery. Collectively, they have performed over 2,500. They are also trained in open surgery should the need arise.
Where is the surgery performed?
Depending on your risk profile and fitness level, it can either be performed as an outpatient surgery at one of our advanced surgery centers or at the hospital in the event that you will need to stay over.
How do you treat bladder cancer?
- Ileal Conduit
- Orthotopic Neobladder
We did not find your search. Please try another entry.
We did not find your search. Please try another entry.
Benign Diseases & Other Conditions

Robotic Total/Partial Adrenalectomy (Functional Adrenal Masses or Adrenal Cancers)

Robotic Retroperitoneal Lymph Node Dissection (Metastatic Testicular Cancer)

Robotic Sacrocolpopexy (Pelvic organ prolapse)
Schedule Your
Surgery Today
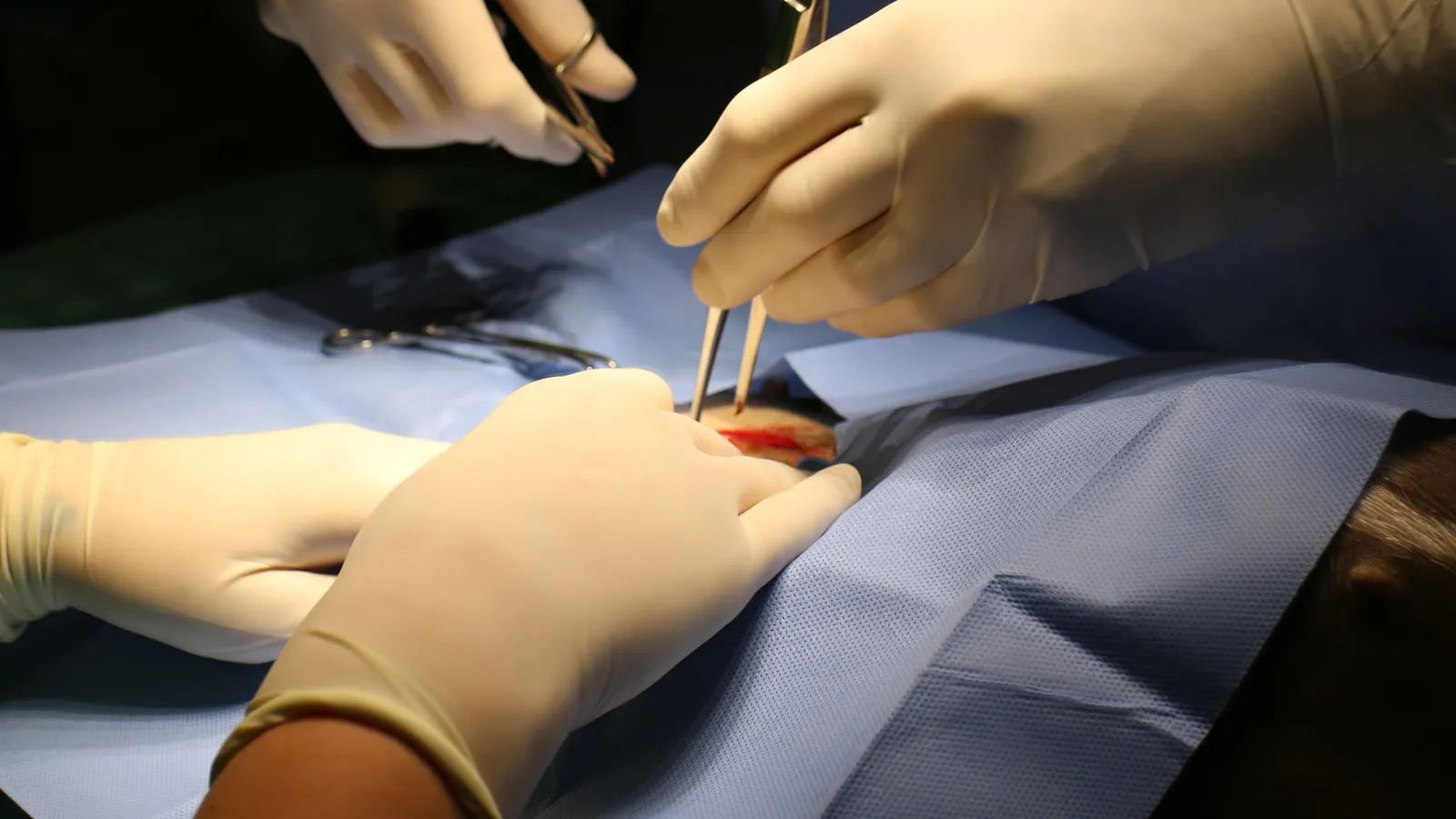
Example of A Robotic Surgery
*Warning: Graphic content